Abstract
Introduction
Core binding factor (CBF) acute myeloid leukemia (AML) inv(16)(p13.1q22)/t(16;16)(p13.1;q22)/CBFβ-MYH11 [inv(16)/t(16;16)] is associated with a favorable outcome in children. Aberrations inv(16) and t(16;16) result in the same fusion of the CBFβ subunit at 16q22 and the myosin-11 heavy chain gene at 16p13, and are thought to share common biological features and outcomes. However, CBFβ-MYH11 fusion transcripts are heterogeneous and may vary in terms of biological activity. Therefore, in this cohort study by the International Berlin-Frankfurt-Munster (I-BFM) study group, we evaluated clinical characteristics, prognostic features and outcomes in pediatric patients with t(16;16)-AML.
Methods
Patients (age 0‒19 years) with cytogenetically or molecularly confirmed t(16;16)-AML, diagnosed by members of the I-BFM study group between 1990 and 2015, were included in the study. Patients with previous malignancies, chemotherapy, or radiotherapy were excluded. Data on baseline characteristics, including cytogenetic and molecular information, fusion type, treatment details and follow up were collected using standardized case report forms. If data on the CBFβ fusion type were missing, real-time quantitative PCR for fusion types A, D, and E was performed on available biobank material. The molecular characterization part of the study is ongoing. Herein, we present descriptive statistics and estimated outcomes related to achieving complete remission (CR) and probabilities of event-free survival (pEFS) and overall survival (pOS).
Results
The study included 46 patients with t(16;16)-AML. Median age was 9.8 [interquartile range (IQR) 1.7‒11.8] years, median white blood cell (WBC) count at diagnosis was 74 [IQR 35‒80] ×109/L and the predominant FAB-type was M4Eo (49%). Eleven patients (24%) had central nervous system involvement at diagnosis. Information on common additional molecular aberrations (e.g. cKIT and RAS mutations) was unavailable for more than 50% of patients and therefore not considered. Information on fusion types was available for 13 patients (28%). Biobank material was used to determine CBFβ fusion type in 2 patients for whom it had previously been unknown. Another 9 samples from international groups are available and pending analysis. Most patients for whom information was available on CBFβ fusion type had type A (n=7, 54%), followed by type D (n=3, 23%) and type E (n=3, 23%). No other fusion types were identified. Patients with type non-A (n=6, 46%) were predominantly male (67%) and had FAB-type M4Eo (83%). They were older than patients with type A (11.9 vs 8.8 years, respectively) and had a higher WBC count (69 vs 48 ×109/L, respectively), but these differences were not significant. Additional cytogenetic aberrations occurred in 38% of patients. Gain of chromosome 8, 21 or 22 were the most common additional chromosomal aberrations. Distribution of additional cytogenetic aberrations was comparable between patient with fusion type A and other types.
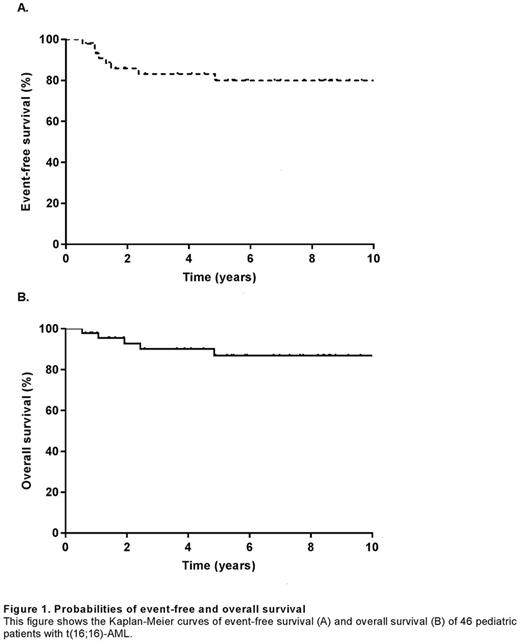
Patient outcome was excellent with a 100% CR rate and a 5-year pEFS and pOS of 80% [standard error (SE), 6.4%] and 87% [SE, 5.6%], respectively (Figure 1). Five patients suffered a relapse. Of them, 4 had WBCs >50 ×109/L at diagnosis. None of the 5 patients had additional cytogenetic aberrations. Two patients had fusion type A and type was unknown for the other 3 patients. Of 46 patients, 2 died after relapse and 3 died from toxic complications in first CR. These complications included failure to recover bone marrow hypocellularity and subsequent multi-organ failure (n=1), and sepsis after stem cell transplantation in CR (n=2).
Conclusion
This is the first report of a relatively large cohort of pediatric t(16;16)-AML patients. Patient outcomes were very good, especially compared with those reported for patients with non-CBF leukemias. However, these patients were at risk of toxic death in CR. Clinical characteristics and outcomes were comparable with those reported previously for patients with inv(16). Although this case series was large, patient numbers remained too small to identify significant prognostic factors associated with outcome. Prospective trials are needed to determine other biological features that may explain differences in outcomes among patients with either t(16;16) or inv(16)-AML.
Kaspers: Janssen-Cilag: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal